Summary: PI-RADS scores assess the likelihood of clinically significant prostate cancer from MRI images. Scores range from 1 (very low risk) to 5 (very high risk) and help physicians decide whether to recommend a biopsy. Biopsies are usually considered at scores of 4 or 5, alongside other risk factors.
Key Points:
- PI-RADS 1–2: Low risk; biopsy usually not recommended unless other risks exist.
- PI-RADS 3: Unclear risk; often followed by more testing before biopsy.
- PI-RADS 4–5: High to very high risk; biopsy typically advised.
- Other Factors: PSA levels, family history, and symptoms also influence biopsy decisions.
- Next Steps: Prostate Laser Center offers minimally invasive, MRI-guided biopsy and treatment options for qualifying patients.
The Prostate Imaging Reporting and Data System (PI-RADS) is a valuable tool used in the diagnosis of prostate cancer.
To put it simply, PI-RADS scores help to quantify the risk level seen in medical imaging of the prostate. Physicians use these scores to help determine the next steps in diagnosis, such as deciding whether a patient should undergo a biopsy on their prostate.
So, how do PI-RADs scores work – what is the scoring system, who assigns the scores, and what do the different PI-RADs scores mean? What happens following the assignment of a PI-RADs score? And when is a prostate biopsy necessary based on a patient’s PI-RADS score?
Keep reading to learn more about PI-RADS scores and their role in diagnosing prostate cancer.
What Are PI-RADS Scores and How Are They Used in Diagnosing Prostate Cancer?
What is a PI-RADS Score?
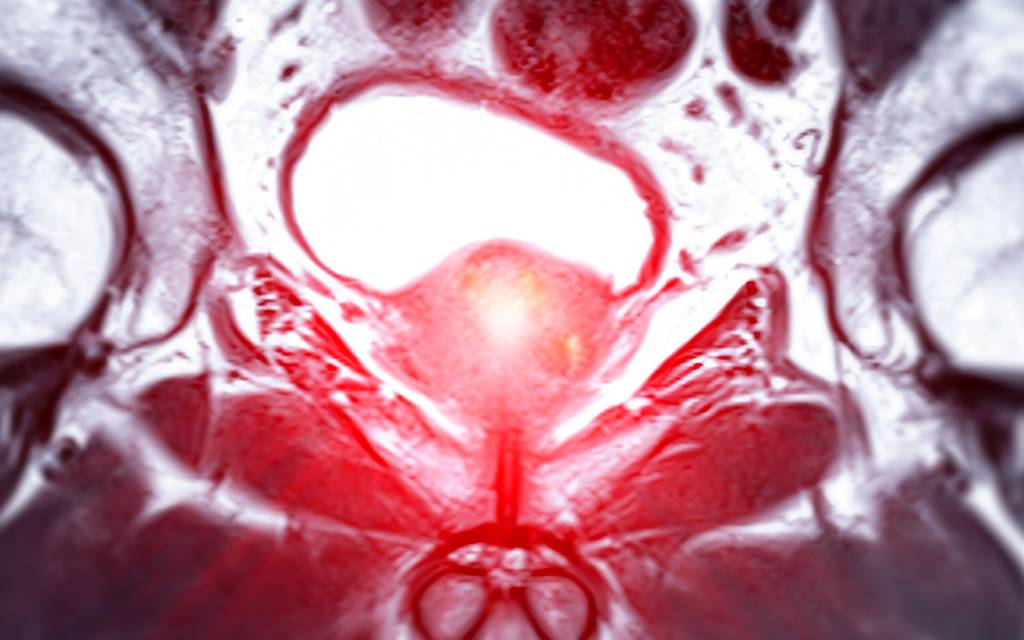
A PI-RADS score is the result of a standardized grading system used by healthcare professionals to evaluate prostate MRI scans – the Prostate Imaging Reporting and Data System. The score indicates how likely it is that clinically significant prostate cancer is present in a patient’s prostate gland and surrounding tissue.
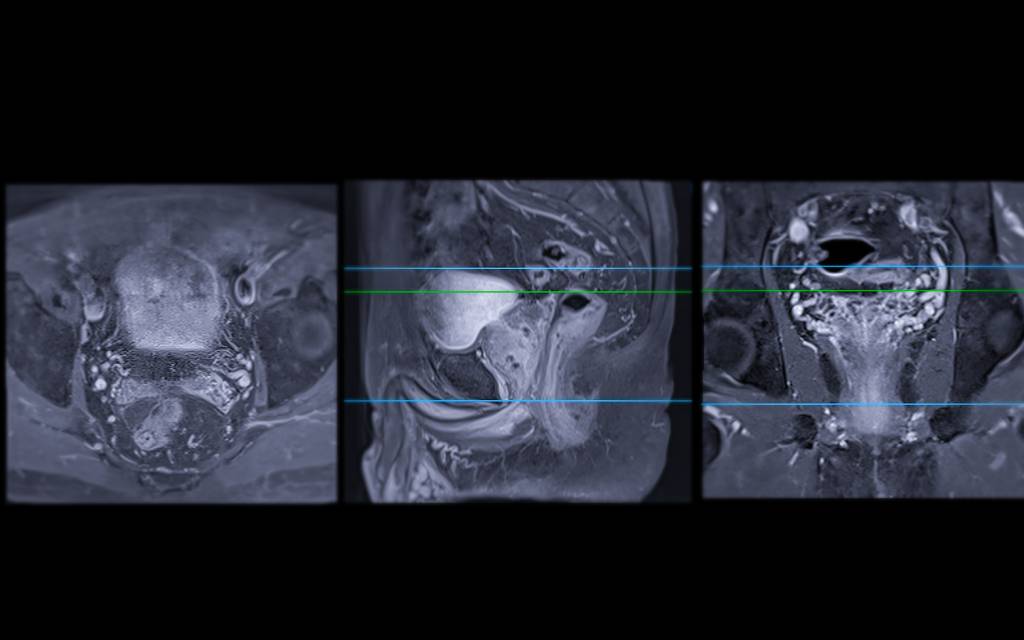
Following an MRI for prostate cancer, specifically a multiparametric MRI (mpMRI), a radiologist reviews the images generated by the scan. These physicians use PI-RADS to score the images because it offers a clear and consistent framework, process, and diagnostic result.
PI-RADS provides guidance for the mpMRI process, directing the use of specific sequences for imaging. It also helps to guide radiologists as they review images by providing context on how clinically significant prostate cancer appears in those sequences.
Because PI-RADS is a standardized system, it makes it easier to communicate risk levels between the radiologists who review the scans and the physicians (including but not limited to radiologists) who treat patients with prostate cancer.
The current version of PI-RADS is version 2.1, which was introduced in 2019. As the peer-reviewed journal European Urology explains, the PI-RADS Steering Committee uses a consensus-based process to identify and correct ambiguities and issues present in the system. This approach leads to enhanced accuracy, improved reporting, and other positive changes.
Abnormalities and areas of concern identified through an MRI do not conclusively prove that prostate cancer is present. Other prostate conditions, like prostatitis and inflamed benign prostatic hyperplasia (BPH) nodules, can appear similar to cancer on an MRI. PI-RADS scores are one of several diagnostic processes and measures used in relation to prostate cancer.
The PI-RADS Scoring System
As for PI-RADS scores themselves, the scale is relatively simple. Radiologists assign scores to areas of the prostate that appear abnormal or concerning, with the score reflecting the probability of clinically significant prostate cancer. The scale is as follows:
- PI-RADS 1 indicates a very low likelihood of clinically significant prostate cancer.
- PI-RADS 2 indicates a low probability of clinically significant prostate cancer, but higher than PI-RADS 1.
- PI-RADS 3 indicates an intermediate or equivocal result – clinically significant prostate cancer is neither unlikely nor likely.
- PI-RADS 4 indicates a high level of risk that clinically significant prostate cancer is present.
- PI-RADS 5 indicates a very high level of risk for the presence of clinically significant prostate cancer.
How PI-RADS Scores Inform Treatment Plans
MRI images and the PI-RADS scores assigned to them give physicians valuable context as they choose how to proceed with a treatment plan. This includes the decision of whether to conduct a prostate biopsy, as well as more precise targeting of the biopsy.
With a low PI-RADS score and other indications that clinically significant prostate cancer is unlikely, the physician may recommend surveillance – regular monitoring – instead of an immediate biopsy. With a high PI-RADS score and other signs of clinically significant cancer, more testing (such as a targeted biopsy) and treatment are likely.
PI-RADS scores are important for building a treatment plan but are not the only diagnostic tool or indicator used. Physicians take PSA levels, Gleason Grade Group, the patient’s current level of health and health history, and other factors into account as they determine how to move forward.
When is a Prostate Biopsy Necessary Based on PI-RADS Scores?
The PI-RADS score assigned to medical imaging by a radiologist is an important factor for determining whether a prostate biopsy is needed, although it’s not the only factor considered by physicians.
Keep in mind that, as the need for a prostate biopsy is reviewed in this section, the PI-RADS score is not the only element that a physician takes into account. A lower PI-RADS score could still lead to a biopsy if many other factors indicate a high risk for prostate cancer.
A high PSA level, and especially rapid elevation of PSA levels across multiple tests, can encourage physicians to schedule a prostate biopsy for a patient. So can a family history of prostate cancer, certain patient symptoms, abnormal findings during other exams, and other potential indicators of prostate cancer.
Also, a physician may instead suggest a follow-up MRI and PI-RADS scoring before ordering a biopsy, depending on the overall picture of prostate cancer risk that diagnostic processes and other indicators show. A physician may also order biomarker testing before scheduling a biopsy of prostate tissue.
While biopsies are not especially complex – most are outpatient procedures – they are still invasive. As the Mayo Clinic explains, bleeding and difficulty urinating can occur following a prostate biopsy. And, while not frequent, a serious infection requiring IV antibiotics, and even hospitalization can occur.
So, physicians won’t immediately move to a biopsy as part of a diagnostic and treatment plan in all situations. Instead, they weigh the benefits and potential risks based on individual patients as they make their decisions.
PI-RADS Scores and Biopsies by the Numbers
All of that said, in general, a higher PI-RADS score is usually a sign that a prostate biopsy is needed. More specifically:
- A PI-RADS score of 1 or 2 means a prostate biopsy is not generally recommended unless other risk factors are present.
- A PI-RADS score of 3 often means that more testing is needed before the decision to conduct a biopsy is made. Remember, because this score is an intermediate result, the risk level is neither low nor high.
- A PI-RADS score of 4 or 5 means a biopsy is usually necessary because of the high level of prostate cancer risk indicated by the MRI for prostate cancer and subsequent PI-RADS scoring.
It is important to note that a negative MRI does not rule out prostate cancer. Even in the setting of a PI-RADS 1 or 2, if there are concerning signs for a possible prostate cancer, a biopsy should still be strongly considered. A high-quality prostate MRI is a powerful tool that can help direct a targeted biopsy when a non-targeted biopsy can miss the cancer. However, no single tool should be overly relied upon.
PI-RADS FAQs and Answers
Have a specific question about PI-RADS scores and related topics and want a clear answer? We’ve listed common questions along with simple and direct answers to them here.
What is a PI-RADS Score?
A PI-RADS score ranges from 1-5, with 1 indicating the lowest risk of clinically significant prostate cancer and 5 indicating the highest risk. Radiologists assign a PI-RADS score to a patient’s MRI images based on standardized guidelines. PI-RADS scores help physicians decide if a prostate biopsy or other procedures are needed to diagnose prostate cancer.
How is the PI-RADS Score Used to Diagnose Prostate Cancer?
PI-RADS scores indicate the level of prostate cancer risk seen by radiologists as they read MRI images of the prostate. MRIs and PI-RADS scores do not conclusively diagnose prostate cancer by themselves. However, they help physicians determine if more testing, including a biopsy, is needed.
At What PI-RADS Score is a Biopsy Necessary?
Prostate biopsies are generally recommended with a PI-RADS score of 4 (high risk for clinically significant prostate cancer) or 5 (very high risk). A PI-RADS score of 3 may leads to additional testing before a biopsy. PI-RADS scores of 1 and 2 in and of themselves do not lead to a prostate biopsy. However, if the patient has a suspicious PSA or PSA trend, nodule on digital rectal exam, and/or concerning family history, a non-targeted prostate biopsy should be strongly considered (if a target is not seen on the MRI).
Can You Have a High PI-RADS Score Without Cancer?
Yes. Some non-cancerous conditions, such as prostatitis and benign prostatic hyperplasia (BPH), can mimic the appearance of prostate cancer on an MRI. Biopsies are vital for confirming the presence or absence of prostate cancer.
How Accurate Are PI-RADS Scores in Detecting Prostate Cancer?
PI-RADS scores are useful and generally effective, but not always completely accurate. Prostate MRI is not perfect (no medical test is), and both false negatives and false positives are possible. The PI-RADS score is an important part of diagnostics but is not the only tool used by physicians to screen for prostate cancer.
Minimally Invasive Treatment Options for Prostate Cancer
Prostate Laser Center provides qualifying patients with minimally invasive, MRI-guided biopsy and treatment options for prostate cancer. Schedule a consultation today to learn if you qualify as a patient and find out more about our approach to treating prostate cancer.
NOTE: The information provided on this website is general medical information and does not establish a physician-patient relationship. Please discuss your particular situation with a qualified medical professional.