Laser Focal Therapy for Prostate Cancer
Prostate Cancer Treatment Options
When it comes to treating prostate cancer, you have many options. The two most commonly recommended choices are radical prostatectomy — a major surgery — and radiation therapy. Because these traditional procedures come with a significant risk of side effects, some patients elect to skip any treatment and take their chances.
There is a tremendous need for a more balanced approach, where the cancer is treated, but with a lower risk of serious side effects than traditional procedures. That’s why we perform laser focal therapy.
Laser Focal Therapy
Laser focal therapy (LFT) can be a compelling option for patients who are candidates.
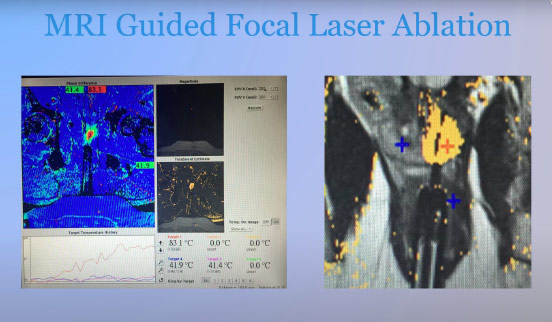
With MRI guidance, we can often localize your cancer (or at least its most dangerous part) to one or two regions of the prostate. We can then place a laser fiber under MRI guidance into those areas.The MRI provides an additional, powerful tool by demonstrating real-time heat maps of the areas of tissue destruction.
Although side effects are possible with any procedure, in appropriate patients LFT can treat the cancer with a lower risk of serious side effects compared to traditional treatments [1-5]. Looking for more information about what to expect?
What is Laser Focal Therapy for Prostate Cancer
Laser Focal Therapy for prostate cancer is a medical procedure that uses the energy of laser light to selectively target and treat localized areas of cancer within the prostate gland. This approach is less invasive than traditional surgery and is aimed at preserving much of the healthy prostate tissue and surrounding tissues, which can reduce the risk of complications and side effects.
The term “focal” refers to the treatment being precisely focused on the cancerous regions, rather than treating the entire prostate. This is similar to how a lumpectomy might be used for breast cancer rather than a full or radical mastectomy.
Who are Good Candidates for Prostate Cancer Focal Therapy
Not all patients with prostate cancer are suitable candidates for focal therapy. Here are some criteria that may make a patient a good candidate for focal therapy for prostate cancer:
- Localized Disease: Focal therapy is best suited for men whose cancer is localized within the prostate and has not spread to other parts of the body.
- Low to Intermediate Risk: Focal therapy for localized prostate cancer is often considered for patients with low to intermediate-risk prostate cancer. This generally includes cancers that are less aggressive and are less likely to spread quickly.
- Well-defined Lesions: High quality MRI helps to identify and localize lesions which helps targeting for both accurate biopsies and targeted treatment.
Patients should have a thorough discussion with their healthcare team to understand if focal therapy is the most suitable option for their specific case.
Advantages of Laser Focal Therapy
Minimally Invasive
A minimally invasive outpatient procedureRelatively Rapid Recovery
Tends to have fewer disruptions to daily life compared with traditional treatment
No General Anesthesia
Uses local anesthesia and moderate, conscious sedation
Decreased Risk of Side Effects
Laser focal therapy for prostate cancer has a lower reported incidence of erectile dysfunction and urinary incontinence than radical prostatectomy and radiation therapy.
Repeatable
If necessary, LFT is a repeatable procedure
No Limitations
If necessary, surgery and radiation are options. “RP [radical prostatectomy] was not complicated by the FLA procedure.” [6]Learn About Prostate mpMRI and Guided Focal Laser Therapy for Prostate Cancer
This video begins by describing the diagnosis of prostate cancer starting with a TRUS biopsy vs MRI. It then describes the advantages and disadvantages of different treatment approaches and provides examples of images from laser focal therapy cases.
Play Video about MRI Guided Focal Laser Ablation for prostate cancer
Frequently Asked Questions
How many days do I need to stay in Houston for an ablation?
What if I need something after hours?
For individuals traveling from outside the Houston area, we can recommend hotels as well as transportation options to help ease your travel planning.
You are provided with both a nurse’s and physician’s cell phone numbers.
Is focal laser ablation covered by insurance?
For Cancer Treatment:
Private insurance will usually not cover a significant portion of the procedure. You can try calling your insurance with these codes and asking: The CPT code is 55899 and the ICD code is C61.
Medicare is complicated, but the answer is generally no.
Do you use the “Blue Laser” for FLA treatment?
Which laser system do you use?
How is your infection rate?
We take many steps to minimize the risk of infection, including an IM or IV shot of antibiotics the day before, the day of, and the day after the procedure.
In addition, we prescribe a course of oral antibiotics. We have patients perform a fleet enema the evening before and the morning of the procedure.
Finally, before starting the procedure, we wipe down the inside of the rectum with betadine to clear any residual debris and wipe down the wall of the rectum with an antiseptic.
Is intravenous conscious sedation safe without an anesthesiologist?
- Performing procedures with moderate sedation without an anesthesiologist present is a safe and accepted practice in the correct circumstances when performed under the supervision of a physician who has completed an ACGME accredited interventional radiology fellowship.
- Our physicians have performed hundreds of procedures with patients under moderate sedation (without an anesthesiologist present), including during complex procedures such as uterine fibroid embolizations, transarterial chemoembolization for liver cancer, ultrasound guided liver microwave ablations, transjugular intrahepatic portosystemic shunt (TIPS) placement, MRI guided laser ablation for prostate cancer, MRI guided prostate biopsies, and more basic procedures such as port catheter or tunneled dialysis catheter placements.
- Having a properly trained physician experienced in conscious sedation and a very high quality registered nurse with significant critical care experience, good judgment, and appropriate certifications (e.g., ACLS, CSRN, etc) is critical. Nurse Donnie has these qualifications.
- Having high quality monitoring equipment including capnography (not required but very helpful) allows moderate sedation to be given even more safely.
- Having the fast acting, IV reversal agents immediately available, along with all the medications required for advanced cardiac life support, intubation equipment, a defibrillator, suction, etc. is both prudent and necessary in the rare event that a situation should arise.
Laser Focal Therapy for Prostate Cancer
Interested in our treatment options?
