Benign Prostatic Hyperplasia (BPH)
What is BPH?
Over the course of a man’s life, his prostate naturally grows larger as he ages. However, if the prostate grows too large, which can sometimes happen in old age, this can put pressure on the urethra and cause some issues related to BPH.
If you’re wondering what is BPH in urology, we’ll walk through what BPH is, how it can affect the body, and what some effective BPH treatments are.
What is BPH in Medical Terms?
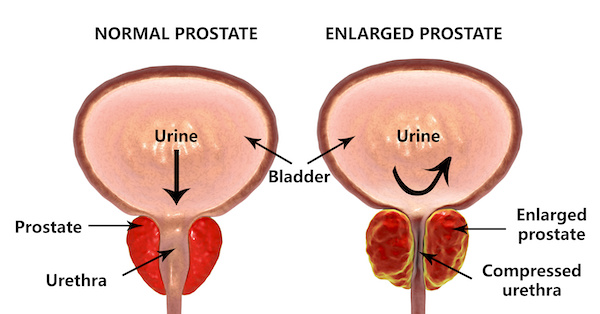
Also known as an enlarged prostate, Benign prostatic hyperplasia (or BPH) occurs when the prostate and surrounding tissue enlarges. BPH occurs as a result of excess tissue growth in the area of the prostate called the transitional zone, which surrounds the urethra.
The urethra is normally closed so we don’t leak, but when we urinate, the urethra needs to open. The excess tissue caused by BPH makes it difficult for the urethra to open, resulting in straining or other discomfort.
The bladder and urethra are essentially a pump and a tube. When the prostate enlarges, it often creates pressure against the tube (the urethra), causing resistance to urine flow. The bladder must pump harder to push urine out against resistance.
Though BPH is benign and doesn’t necessarily lead to anything more serious, the symptoms of BPH can be uncomfortable and start to disrupt daily life. This is where treatment can help.
What are the Symptoms of BPH?
Men with BPH may experience different BPH symptoms, including:
- Difficulty urinating
- Straining to empty the bladder
- Nocturia (or waking up at night to urinate)
- A weak stream
- Delayed onset of urination
- Starting and stopping the flow
- Incomplete emptying
- sometimes urinary tract infections.
Why Doesn't the Bladder Empty?
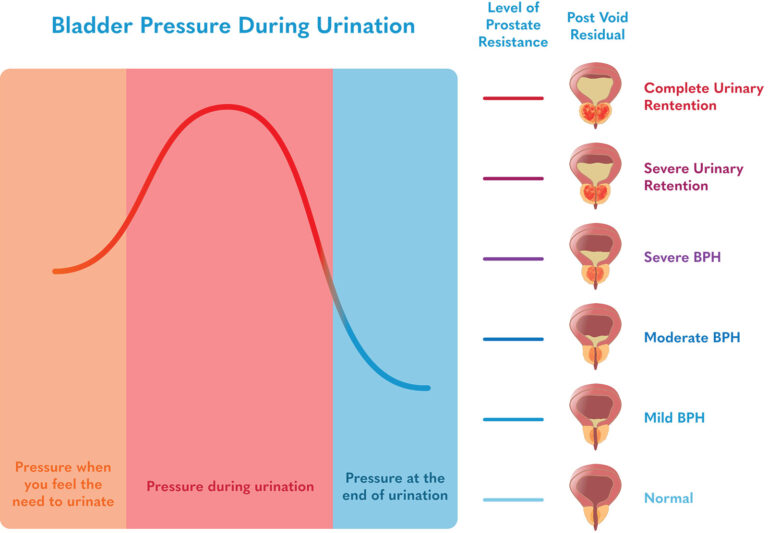
The worse the BPH, the more residual urine remains in the bladder after urinating.
Initially, when starting to urinate, the pressure increases within the bladder. During urination, the pressure peaks and then gradually decreases. When the pressure of urination matches the level of resistance within the prostate, urination stops, and whatever urine is within the bladder remains. We call this post-void residual.
Because stagnant urine is prone to get infected, men may start getting urinary tract infections (UTIs) for the first time as they deal with this problem. Generally, once the post-void residual is greater than 100cc or ml, the bladder begins to suffer irreparable harm.
Treatment may partially reverse bladder damage, but more importantly, it will usually prevent further bladder damage.
BPH Treatment Options
When it comes to the treatment of BPH, there are a few different routes you can take.
Medications for BPH
BPH is usually treated first with a medication called an alpha-blocker (Some examples include Flomax, Alfuzosin, and Rapaflo). These medications help to relax the muscles in the prostate, taking some of the pressure off the urethra. Unfortunately, these medications often have side effects, including dizziness, decreased energy, and/or retrograde ejaculation. Consult with your doctor before starting any of these medications.
Another class of medications is 5α-reductase inhibitors (e.g., finasteride or dutasteride). These medications block the body’s production of a version of testosterone that causes the prostate to enlarge. As a result, they can also decrease erectile function, energy, and libido.
Traditional Procedures
A transurethral resection of the prostate (TURP) is commonly used as a treatment of BPH. With a TURP, a camera and cutting device are advanced into the penis. The prostatic urethra and the internal urinary sphincter are carved out and the urologist will continue cutting out tissue until he or she feels an adequate amount has been removed.
While this is an effective procedure, some men experience erection difficulties and many men experience difficulty with ejaculation after. One study found that 5.8% of patients with previously good sexual function, reported a worsening of erectile function, and retrograde ejaculation was reported by 48% of those sexually active after TURP. Additionally, the procedure has a significant risk of bleeding with an average blood loss of approximately 500cc.
Because of the large amount of blood loss associated with TURP, the GreenLight Laser was developed. It is very similar to a TURP, except that instead of using a cutting device, a very high-powered laser is used to literally vaporize the prostatic urethra and tissue beyond.
This allows the GreenLight Laser to generally have less blood loss than a TURP, but still much more than a minimally invasive procedure.
Minimally Invasive Procedures
To minimize the risks of BPH treatments, Prostate Laser Center offers two minimally invasive procedures: Laser Focal Therapy and TULSA-PRO. Both procedures may be relevant options for BPH treatment without some of the risks of traditional treatment. . Laser Focal Therapy uses an FDA-approved laser system to insert a 1.85-mm laser fiber through your rectum into your prostate under MRI guidance. By monitoring the laser energy in two different planes in real time, the physician can see the neurovascular bundles responsible for erectile function and ejaculatory ducts to avoid harming them.
This laser system is so precise that it’s most commonly used in the brain. There are no guarantees in medicine, but this system minimizes the risks to your neurovascular bundles, internal urinary sphincter, and prostatic urethra. With this treatment option, retrograde ejaculation risk is about 15%, and the risk of erectile dysfunction is less than 5%.
The TULSA procedure (TULSA-PRO) ablates prostate tissue from the inside out. A device enters the urethra which delivers thermal ultrasound energy outwards from the urethra to the prostate while under real-time MRI guidance.
This approach avoids the need for surgical incisions to reach the prostate. A cooling mechanism helps protect the urethra from ultrasound energy. The thermal ultrasound energy is delivered in a sweeping motion (visualize a clock hand sweeping), which enables the physician to ablate a wide area.
Though both of these BPH treatment options can be effective for some people, every man is different, and so are their prostate concerns and best treatment options. If you think you’re experiencing BPH and want to explore one of these procedures offered by Prostate Laser Center, fill out the form below to request a consultation.
The Anatomy of BPH
The bladder and urethra are essentially a pump and a tube. When the prostate enlarges, it often creates pressure against the tube (the urethra), causing resistance to urine flow. The bladder must pump harder to push urine out against resistance.
Seeking treatment for benign prostatic hyperplasia (BPH)?
Request a Consultation
