TL;DR: The TULSA procedure (TULSA-PRO) is a minimally invasive prostate cancer treatment that uses MRI-guided ultrasound to ablate cancerous tissue. It has a strong success rate and a lower risk of long-term side effects like urinary incontinence and erectile dysfunction compared to traditional surgery and radiation therapy. While generally well-tolerated, short-term effects like urinary urgency and discomfort can occur.
- Short-term effects: Temporary urinary urgency, discomfort, and rarely infections.
- Long-term risks: ~8% urinary incontinence and ~25% erectile dysfunction.
- Compared to other treatments: Fewer side effects than surgery and radiation; somewhat more than laser focal ablation.
- Popular for: Preserving urinary/sexual function and offering repeatable treatment.
- Ideal for: Low- to intermediate-risk cancer localized to the prostate.
Learning about potential options for treating prostate cancer empowers patients to make more informed decisions about their personal medical needs.
Of course, consultation with a physician is always crucial. These discussions take personal medical details into account and offer a level of specificity that general information can’t provide. However, researching potential treatments can give patients more context to use during those consultations and when choosing how to move forward.
Among minimally invasive procedures for prostate cancer, transurethral ultrasound ablation (TULSA-PRO) has emerged as a medically proven and effective treatment option. It can perform especially well when patients have a larger cancer or a more diffuse cancer in the prostate gland.
As with every treatment for prostate cancer, there are side effects to consider as well. Keep reading to learn more about what TULSA-PRO is, the potential side effects that can occur due to this treatment, and a comparison of TULSA-PRO side effects with the side effects of other options for treating prostate cancer.
What Is the TULSA Procedure?
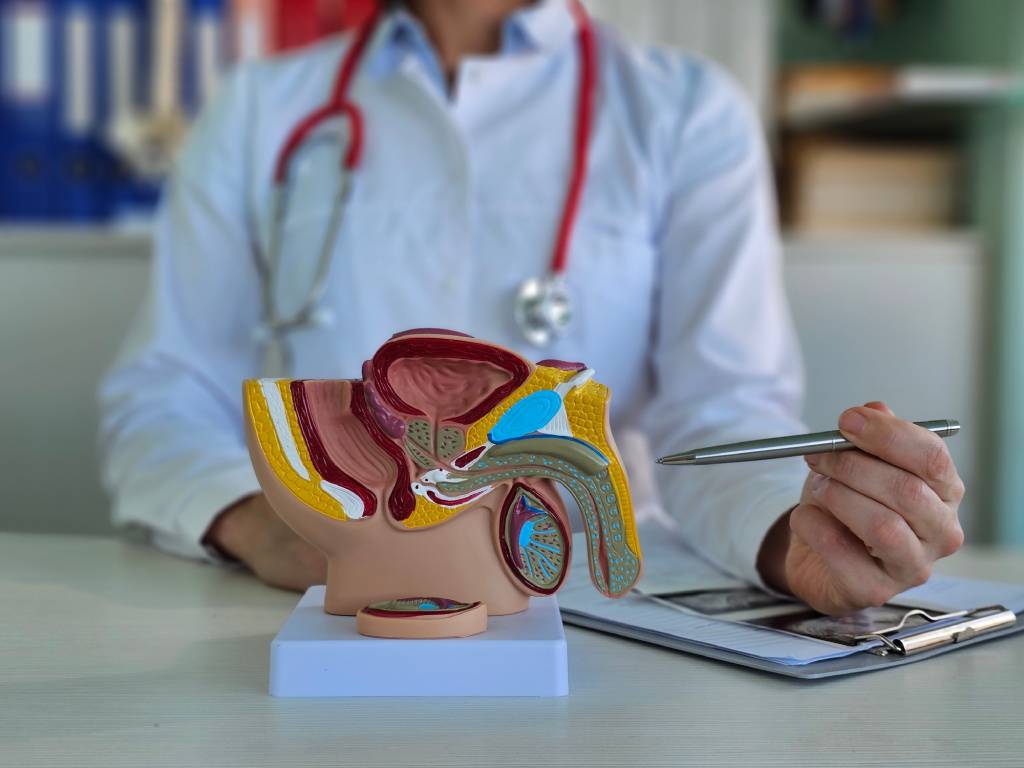
TULSA-PRO stands for transurethral ultrasound ablation procedure, a minimally invasive procedure used to target cancerous tissue within the prostate. Here’s a more in-depth review.
Key Information About TULSA-PRO
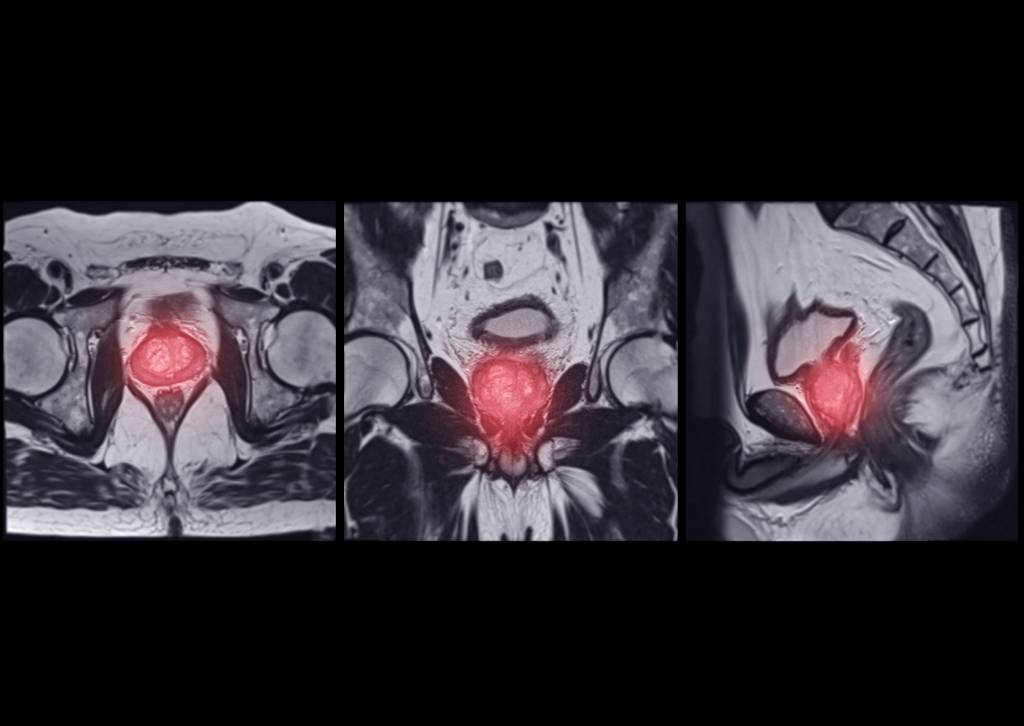
TULSA-PRO prostate treatment uses directional thermal ultrasound energy to ablate (heat up and destroy) cancerous and other unwanted tissue in the prostate. The patient is placed under general anesthesia, and a small device is inserted into the urethra to emit the ultrasound energy, along with an endorectal cooling system.
The area is mapped using real time MRI, the treatment plan is determined and confirmed, and the TULSA-PRO system begins the process. The physician receives frequent updates through imaging, directing, and adjusting the process as necessary for both patient safety and effectiveness. This approach helps to preserve urinary and sexual function.
A key factor in the delivery of TULSA-PRO treatment is the feedback provided by real-time MRI guidance, which allows the physician to carefully target affected areas and adjust the delivery of ultrasound energy in real time if needed. The cooling mechanism helps to protect sensitive structures in this area of the body, as procedure developer Profound Medical explains.
TULSA treatment for prostate cancer also uses robotically driven delivery, enabling both precision and broad tissue destruction.
TULSA-PRO is commonly used to treat prostate cancer that is more diffuse or larger but still within the prostate gland itself. However, TULSA-PRO is also employed to treat issues such as benign prostatic hyperplasia (BPH), using ultrasound to destroy excess (but not cancerous) tissue.
One more key advantage of TULSA-PRO to note, in comparison to certain other treatment options for prostate cancer, is the preservation of treatment options if needed in the future. Patients who require further prostate treatment can repeat TULSA-PRO or choose any other type of prostate therapy that aligns with their needs.
The TULSA Procedure for prostate cancer is normally completed in a single session and is an outpatient procedure. TULSA-PRO side effects are covered in greater depth later on in this blog. However, in general, TULSA-PRO offers lower instances of certain post-operative side effects as compared to radical prostatectomy (removal of the prostate) and radiation therapy.
TULSA-PRO Success Rate
In terms of the procedure’s success rate, research published in the peer-reviewed Journal of Urology found that:
- In a controlled study, 85% of 111 participants who underwent TULSA-PRO were free of cancer that scored in Gleason Grade Group (GGG) 2 and above one year after treatment.
- Additionally, 79% of participants were free of GGG 2 and high-volume GGG 1 disease.
Who Is TULSA-PRO For?
Patients need to consult with a physician to determine if TULSA-PRO is an appropriate treatment option on the individual level. That said, TULSA-PRO is generally used to treat relatively healthy men who are able to undergo general anesthesia with:
- Low- to intermediate-risk prostate cancer.
- Cancer that is confined to the prostate.
- A PSA of less than 20.
Why TULSA-PRO Has Gained Popularity
TULSA-PRO has increased in popularity since it emerged as a new prostate procedure because it:
- Requires no incisions and, in most cases, no overnight hospital stay.
- Offers enhanced precision through MRI-based planning and monitoring.
- Is designed in part to help preserve urinary and sexual function after treatment.
Common Side Effects of TULSA-PRO
On a practical level, TULSA-PRO side effects can be divided into two distinct groups: mild and temporary side effects and less-common, persistent side effects.
Mild and Temporary Side Effects of TULSA-PRO
TULSA-PRO can lead to urinary frequency or urgency above what a patient considers normal following treatment. This issue tends to resolve itself within a few weeks as the body heals.
Pain and discomfort in the ablation area are seen in some patients. These issues also tend to resolve as the body returns to normal following treatment. Blood in the urine and urinary tract infections (which can be managed with medications as part of post-operative care) are additional short-term side effects. Infections are not particularly common, but are possible.
Urinary retention following the removal of the urinary catheter used in the short term after treatment is possible as well. This TULSA-PRO side effect can also be managed by a patient’s care team.
More Significant, Less Common TULSA-PRO Side Effects
It’s important to be clear: Some TULSA-PRO side effects have a lower incidence as compared to other types of prostate cancer treatment, such as radical prostatectomy and radiation therapy. However, TULSA-PRO treatment still has potential long-term side effects for some patients.
Selected clinical trial data for TULSA-PRO, along with follow-up data, were shared by AUA News, the news outlet of the American Urological Association. The two major TULSA-PRO side effects identified were:
- Urinary incontinence: About 92% of men who underwent TULSA-PRO treatment were pad-free five years after treatment. This means only about 8% of patients needed to use urinary pads and similar items because of a loss of urinary control.
- Erectile dysfunction: Roughly 25% of patients experienced grade 2 erectile dysfunction five years after treatment. Keep in mind that grade 2 erectile dysfunction can generally be treated with medication and medical devices. More rarely, there can be erectile dysfunction that does not recover with medication.
How TULSA-PRO Side Effects Compare to Other Prostate Cancer Treatments
TULSA-PRO vs. Traditional Surgery (Radical Prostatectomy)
TULSA-PRO side effect rates compare favorably to those of traditional surgery, specifically a radical prostatectomy, for prostate cancer. In addition, TULSA-PRO is an outpatient procedure that can offer a faster recovery time as compared to the inpatient radical prostatectomy.
As noted previously, TULSA-PRO has a urinary incontinence risk of roughly 8% and a roughly 25% risk of erectile dysfunction.
Radical prostatectomy has a urinary incontinence risk of about 16%, according to research published in the journal European Urology. Risk related to erectile dysfunction varies. However, a review published in the journal Current Opinion in Supportive and Palliative Care suggests an approximate risk of 50%, about twice that of TULSA-PRO.
TULSA-PRO vs. Radiation Therapy
Radiation therapy is a traditional prostate cancer treatment that uses radiation to damage cancerous cells, stopping or slowing their growth. It can be a recurring outpatient procedure, as is the case with external beam radiation therapy, or an inpatient procedure when brachytherapy (targeted implantation of radioactive material) is used.
The risk of urinary incontinence posed by radiation therapy varies, but it is roughly 10-18% according to research published in the journal Urologia Internationalis. That’s higher than the risk of urinary incontinence posed by TULSA-PRO.
In terms of erectile dysfunction, the risk posed by radiation therapy is also a range. Research published in the Journal of Sexual Medicine set the range of erectile dysfunction side effects at 34-57%. The erectile dysfunction risk for TULSA-PRO is about 25%.
Radiation therapy often also requires the use of hormone therapy (a polite way of describing chemical castration) which also has its own list of side effects.
TULSA-PRO vs. Laser Focal Therapy
Laser focal ablation (LFA) is a minimally invasive, MRI-guided treatment option that, similar to TULSA-PRO, is designed in part to preserve healthy prostate tissue and surrounding tissue.
While both offer precision in terms of treatment, laser is probably more precise than TULSA-PRO. One practical comparison is the coverage of a roller brush (i.e. TULSA-PRO) vs a paint brush (i.e. laser) when painting a wall. Laser is generally used for patients with more focal disease or disease that is in a more sensitive location (such as next to a nerve bundle).
LFA and TULSA-PRO can be used together in some cases. For example, when cancerous tissue near a nerve bundle and present throughout the prostate, LFA can be used to target cancerous cells near the nerve bundle while TULSA-PRO is used to vastly widen the margin throughout much of the rest of the prostate.
Research results from the Phase II trial of LFA for prostate cancer, shared by UroToday, found that this procedure has:
- A urinary incontinence risk of about 3%.
- An erectile dysfunction risk of less than 10%.
Finding Prostate Cancer Treatment That Aligns With Individual Needs
Prostate Laser Center offers minimally invasive treatment options for prostate cancer, including LFA and TULSA-PRO. Consulting with a physician will help you understand the treatments for which you qualify.
To learn more about LFA and TULSA-PRO treatment and if they are appropriate for your needs, request a consultation today.
NOTE: The information provided on this website is general medical information and does not establish a physician-patient relationship. Please discuss your particular situation with a qualified medical professional.